Patient, patient
CHANGER DE PERSPECTIVE(s) À TRAVERS LE TEMPS
(Description traduite avec Deepl.)
Ceci est un montage d’une conversation avec Al Versieux le 24 juin 2024. Il s’agit d’un instantané de ce à quoi les perspectives temporelles peuvent ressembler dans le contexte d’une maladie chronique et terminale. Elle a été enregistrée avec des sous-titres automatiques dans le logiciel de vidéoconférence open source BigBlueButton (BBB), puis éditée en un texte quelque peu cohérent. Certaines parties du texte ont également été transcrites en audio, parce que notre anglais était devenu trop flou et que les sous-titres BBB ne pouvaient pas nous suivre, ce qui explique que vous puissiez parfois voir des indications de temps. Nous avons divisé la conversation en 7 parties.
Parts:
Intro -
Part 0 - Before
Part 1 - Six months
Part 2 - Imagining medicine
Part 3 - Next
Part 4 - Two thousand and fifty one
Part 5 - No
Part 6 - One week
Part 7 - Limbo
Intro
Yeah let me see where it goes,(yeah go ahead)
It’s nice,
but also,
the typical mind yoga.
(Yes,
huh!)
So,
we talked a bit…Yeah now i dunno,
we can just start somewhere and talk a bit?
some time ago we talked a bit about time perspective, and what the knowledge of a successful patient is, they are kind of two different topics,
but i dunno where to exactly start.
From my perspective, of being given different timelines, or even like, when you’re also the one who has to kind of set a timeline because the people who are there to guide you don’t actually know exactly where you’re going.
Like the limbo limbo limbo that it is, a blurry time somewhere.
Part 0 - BEFORE
Before I knew I had cancer I only knew something was going on, so I went already to do a lot of medical exams during one year or something. But when you don’t know what you have, you start to go to see a lot of different doctors and specialists, like gynecologist, pneumologist, etc. I get like a lot of technical exams, like echography, scanner and all that stuffs. But nobody gave me a real diagnosis and I had still pain in my body and one night I woke up with a huge neck so that I couldn’t move my head anymore.
So the moment when I was going to my first little hospital and they finally said okay we know what you have that was a big moment for me, like at that moment I was like okay! Now that we know, we can start something.
And after that, came a change of speed.
The doctor said we don’t have a final solution for this.
Well, then I got concerned.
Part 1 - SIX MONTHS
I’ve been in many limbos,
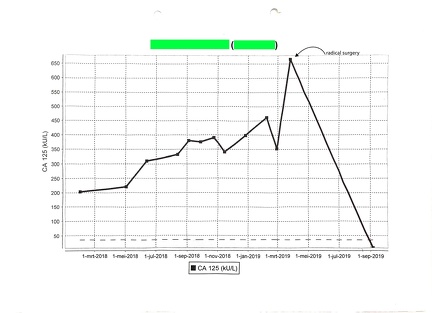
For me the first limbo was when they gave me six months to live. I was twenty eight years old. sometimes, the time is also to remember, I try to remember really, I can remember days, I know that they said it to me on the twenty six of December two thousand and twelve, that they told me that i have an ovarian cancer stage 4B (https://cancer.ca/fr/cancer-information/cancer-types/ovarian/staging) with tumour of 10 centimeter on the ovary and metastases in the peritoneum, pleura and neck lymph nodes.
But now it is eleven years and a half after this six months limbo. that’s a long time now
So all this time is passing, and this thing comes back to me a lot, years and years have passed after they gave me six months.
And, and sometimes in a sentence or two I understand that many people I know don’t know about it, people that I’ve met just now don’t know my medical past and, yeah, what I’ve seen and and what I went through and what I’m still experiencing.
When you’re given different diagnoses over the years, they are also like different expected timelines and different reads of a situation.
Like, you’re being told you’re in different situations. This also happens because they just don’t know. When they don’t know what to expect and don’t have a miraculous solution for a patient ,and decide to just try something instead. Because anyways each cancer is specific to each person, your body reacts in a different way, or you don’t have the same organs and it all works differently. For example, I knew that my liver was in really good shape from the beginning and probably that helped me a lot.
So they try to guess it but they don’t know, they try to give a kind of amount of time that you can survive if you have
taking this type of cancer
plus the age, i was twenty eight years old,
plus the medical condition
they wrote a concept and after tried to calculate more more or less how many months, years do you still have,
it is a limited system, so you can end up outside or beyond their spreadsheet. And you start to navigate through all of this with no perspective of time.
There:
x x x xxx xxxxxxx
x x xxxx
xxxxxxxx xx
Like for example, in the first limbo where they gave me six months, I guess the purpose of giving this timeline is that they give a certain orientation or to give someone something to work with, it’s supposed to help like okay now I know the severity and I can work with this. But then surpassing all those estimates and also by so much it’s maybe doing the opposite, it can be disorienting.
You’re, you’re, you’re beyond all of them and you’re off the spreadsheet.
They told me there was no medication enough strong to kill my cancer, so at that moment there are a lot of questions entering your mind, am i going to survive? they gave me only six months so why do i have to try? why do i have to live?, but then i had to leave behind this kind of questions.
Just to give way for a perspective.
Surely if you don’t do that, then you go completely into a depression.
Or, maybe not, I’m not sure we’d know.
But maybe I wanted to somehow be outside of the spreadsheet to ensure that
no, i will not die.
It’s not my time.
I was always like:
No, there isn’t a possible reason here.
This is nuts.
But this is happening.
There is the possibility that in six months yeah it’s finished for me.
No, i want to see further ….
all the moments that I was doubting,
maybe they are right?
But all the time I renegotiated.
So, there are the six months, but also an after:
News, I’m still there.
Part 2 - IMAGINING MEDICINE
One day, after the first six months of the first diagnose, in my first hospital, they said we can’t do anything more for you, we don’t have anything anymore to give you.
Because there was no specific medicine for me actually at that moment, there was no medicine for people with an ovarian cancer, even when they started my first chemotherapy, it was a chemotherapy for people with breast cancer.
They said to me if you were coming one week after the day that you came with what you had, we don’t even know how it was possible that you survived until now, and you wouldn’t even have been told to start the chemotherapy. But my time in this hospital was finished after the six months chemotherapy because they didn’t have anything else to offer me.
As i couldn’t possibly stay with a perspective like that, through the mother of a friend, I found my super specialist who followed me from there on. He retired three years ago, but yeah it’s also a long time that he’s been with me, seven or eight years. And he said to me, really since the beginning,as long as you’re sick I will never let you not have any medication. I don’t know how many years it will be but I will always find something to give you and so through saying this he gave me a kind of a new perspective.
So they started to imagine something for me, a kind of combination of chemotherapy and what they were doing at that moment, eleven and a half years ago.
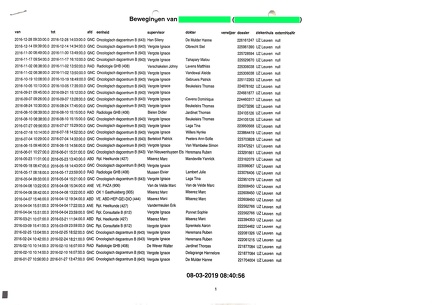
And from that day, i was always following/entering a new protocol, a medical protocol. There’s a lot of practical instructions. Or a reality that gets constantly reset for you.
For the last eleven years and half , i have been on a lot of medical trials, such as chemotheapy by the belly, or surgery of umbilical and inguinal hernia, I also went a lot to the emergency, with a lot of pains and agony, and a lot with side effects that we didnt know how to deal with, staying in a bed waiting for it to become better, i received several peridural treatments, i stayed a lot waiting in hospital, on a chair, in a room, in a bed, in front of doctors, trying to understand the whole medical language, …
Part 3 - NEXT
You are always looking for the best perspective of treatment but how to choose between incertainities?
In July two thousand thirteen, one hospital I contacted in Paris, offered a three month full recovery plan, saying that we do a complete removed surgery and after that you will take a little bit of chemotherapy and after that all is fine.
At the same moment, my specialist said that this is really not a good choice, because they can’t guarantee you full recovery through a surgery, what they offer you does not seem possible.
So I had this impossible choice to make because how do you know if what you choose will be the best for you and that you don’t take the decision that will kill you, or entering in a long process of protocols, clinical trials with no ending time or you can enter now in a promesse of a surgery and take some medicines for some months and after all fine for you.
I know my case, and this offer was even discussed in an international meeting where cancer specialists from different countries meet to share and compare situations.
My (actual) university hospital said:
We will never go on your body if we don’t think you can have a complete recovery, and only if we can’t do it any other way.
We’re especially developing medicine for people with ovarian cancer, and if you want you can enter this medical trial.
With them, I could enter into the trial straight away in a month, so I chose into this long process of protocols and clinical trials.
21:56
They said we will always have a clinical trial in a drawer for you but we need to find a pharmaceutical laboratory who wants to follow us on that.
yeah at the end, it’s all about money to be able to develop medicines.
I mean, I always choose the university hospital because I had more trust, it was a feeling, and also they were more like in the vision to develop medicine for the future. so i decided to follow that.
So he said for a certain amount of time, to not let you without any medication, we let you first on a medicine that is already developed but not done for people who have an ovarian cancer and maybe in six months if we receive the money of the pharmaceutical laboratory, we will try a new one.
it was July two thousand thirteen,
actually six months more or less after the diagnosis.
After that, my first hospital said we cannot do anything more for you at this point,
in April two thousand thirteen, i had my first appointment in Leuven, in this university hospital,
to start already to think of what’s next for me, but you need to realize that you do that also when you are like super sick, on chemotherapy side effects, etc. There is also a bunch of administrative things that you actually have to go through while you’re doing this because it’s a complete life change, i was at that time living and working as a stage manager of a theater and concert place in Paris since three years, my life was somewhere already so i had this impression that i had to do a stop and rewind. I needed daily help for going through the chemotherapy, because you can do nothing alone, you can’t even go out of the bed or preparing your food, or…… and I had to move home to Belgium for more support like coming back to my mother’s place.
The other important administrative thing that i needed to think, to secure for my possible future , was the money, because i was employee, i had a salary but after i was invalid and so not on the job market anymore (as they say) but you must do a lot of calls and papers to understand and also think fast even if people say that you have six months to live because if you don’t do it now maybe if you are still alive on medication, you will not have money every month.
I had to spend some of those time in the six months preparing for surviving even if i didn’t know if i will survive.
At the beginning when they diagnosed me at the hospital, some days later they started the chemotherapy so i stayed in the hospital for some weeks and after i came back home and every two weeks i was going to take chemotherapy at the hospital. From the moment you take it, for the four-five-six days after, you are completely out of life, you just need to try to think that everything will go better after. And then you can start to think that you can call all the administrative institutions to try to understand and to try to have an invalid status between Belgium and France. And after hop, you start again, you go back at the hospital and take again your chemotherapy.
I spent a lot of time to call to understand how it works and how can i have the social security support.
During that period of six months to live, i was also still going in Paris and trying to still have a foot in the theater place and theater companies with who i was working.
And i was also trying to understand how is it possible to live from the social security with 500euros per month. So while i had a conversation about that with a friend in a bar in Paris, the barman told me to try to ask at my last work to have an invalidity pension supplement from their social security. I didn’t know that was existing, nobody from all the administrative people that i had on the phone told me about that.
Maybe it is this also that helped me to survive, trying to plan a future in a way.
Part 4 - TWO THOUSAND AND FIFTY ONE
It’s called an invalidity pension.
at the beginning you start with something else for three years, it is called a daily pension because you are not in a long term diagnosis. They wait three years to say ‘ah you are still alive, so we can put you on an administrative status that is less painful for you administratively.’
This timeline is a little bit crazy, so i remember that one day in two thousand fifteen, two years and a half after i started to do this whole administrative process, i received a letter that was telling me that i would have this invalidity pension supplement from two thousand fifteen until two thousand fifty one, so for thirty six years.
wow
imagine,
I don’t even have an idea of how old i will be in 2051.
I’m from 1984 so, fifty one sixty six
sixty seven
yeah yeah,
pension, maybe it is based on my working age,
yeah yeah yeah yeah
and then probably when you’re going on pension, i will receive something else,
but i have no idea,
maybe i need to already think about that that i need to ask okay what will happen after 2051
because actually i will not have pension?!
and if I’m still alive at that age, what does it mean?
did they already have a person in their system with an administrative status like that? how has it been given to someone who has bypass that age or like that that year,
33:07
Mia: how does that yeah how does that feel to receive that because yeah how,
how does it feel?
al: At first I thought maybe they made a mistake on the paper because it looked like they swapped the numbers 15 and 51, and then somehow I felt safe, because it meant the money would come every month until my doctors said I could work again. Also it was meaning that I didn’t need to ask my family or friends for money.
it is bizarre to have one specific date but it also changes the time perspective, there is a perspective somewhere,
It’s maybe possible then to go until there, that age,
35:11
Mia: yeah but it’s interesting way to see it though because you’ve had this experience of being handed these different dates, to accept, you know from six months very close to like than two and a half years later-three years later, you’re sitting with a paper that is telling you, you have this pension until two thousand fifty one, you know it’s quite a contrast
between the two papers with the two messages.
al: yeah
and i guess,
i wonder, i mean,
like what you said earlier like maybe with the,
the first time
with the six months to live, you couldn’t sort of accept it or you didn’t put too much weight on it or like you didn’t accept that as as a reality,
but sort of … no no no, because it was like; that it is not possible. And i saw also my family around was really what the fuck is happening now? And some people where calling me saying like it is not an ovarian cancer that you have, i saw on internet that or that …
for sure you will live…
yeah that’s, yeah, i think i didn’t want to understand, this is for sure, allez, for me it was really not a possibility that, allez, i didn’t understand how it was possible to have this cancer in me, the moment that i had the more pain was when they were giving me medicines,
it’s not that i really felt the tumor or what i had inside all the time, on some moments, yes for sure, but it is more when they were putting something in me, the chemotherapy is really going everywhere to kill metastasis and tumor but also your good cells, and at that moment you feel really the burning inside your body, pain in the intestines or the belly, and also difficulty to breathe, you loose weight, hairs, all the hairs that you have on your body, etc.
So then it was like, no, how is it possible that i have this thing? This reality to have six months was like no no, i will find another doctor and we will find another solution and maybe i had also more trust in the medical system at the moment, that the doctors are doctors and they know,
yeah
but when i discovered that actually they don’t know and don’t have solutions,
they just try and that you become really like the trial patient
yeah
there you understand that you need to find other ways, and i went a lot in the complementary medicine as traditional chinese medicine, healers of all kinds, etc. also to heal or to try to heal. No actually, to care for your disease and that not all the answers will be in this ‘occidental’ type of medical system, because they never say that you will heal, maybe after 10 years of no activity of the cancer, they will say that you are on remission,
but for the medical system, the cancer will always be inside you, and maybe one day it will wake up, so it stays in your head and stresses you all the time,
yeah
Part 5 - NO
It was seven years after my diagnosis, on the twenty sixth of March two thousand nineteen.
Also on a twenty sixth of the month.
That’s true. five years ago.
My specialist said now we have a problem; we need to go on towards surgery, this medicine is not seen as an interesting financial project for the pharmaceutical laboratory anymore.
Because this last clinical trial, I did it for more or less three years every month or two i needed to go in the hospital to take it. We were at the beginning like forty patients in the trial but on the last year I was almost the only one left with another patient in Spain.
They said to me ok we need to stop the medicine because the pharmaceutical laboratory doesn’t want to put money anymore in this medicine because you two are the last patients who take it. It is not financially interesting for them to develop that medicine anymore.
And I remember I was taking this medicine through my veins on my seat at the hospital when they were announcing that to me and to finish the complete trial i needed to come back one last time but i had planned to go skiing and i was like do i cancel that? and i was so pissed off at the pharmaceutical lab holding this power of money where they were able to just say we stop it and we don’t care about you even if this medicine is more or less working during three years and that the pharmaceutical lab had no proposal for me after … i said i will not come back to finish your trial. fuck off. if you don’t consider me as a human, i don’t consider your trial neither. And then they continue to tell me it is important I still finish the current trial and take the last doses,
but I said no.
and so yeah i knew that i was entering in a new blurry time.
Mia: yeah it looks like every time something comes to an end, you know that you’re going to go into a new protocol, a new reality in a way.
Part 6 - ONE WEEK
42:38
They say okay, so, we will schedule your surgery.
This was the surgery that they always said that it will not happen and that they didnt want to do until there is nothing, nothing, nothing, to give me anymore, as treatment and that was the moment.
So it meant that if the surgery will work, and there was only like really a tiny, tiny chance that I will survive in a way. And if it doesn’t work; i may not wake up, which means dying. Or i will wake up from that surgery maybe in a state worse than before because a surgery is a surgery, and this is a big surgery. It can be that i have complications.
In these scenarios, or in the choices I make, the doctors didn’t give me a clear future scenario.
Mia: yeah then you have played your final card in a way
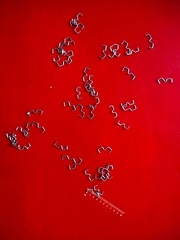
al: they called me to schedule the surgery one week ahead. So it means that I had
one week to do
all the things that I wanted to do in all my life.
In that period, i asked my friend, who is oncologist; and what if i had said yes 6 years before at the surgeon who wanted to do a surgery on me? he said to me dont think about that, just think about now, and that the choice you did brought you to be alive.
Mia: I remember something from that week
a paper
a paper you drew and wrote with everything you wanted to do
al: It is super difficult, also to understand what you always wanted to do, because one week is actually not a long time.
yeah
even if you want to go to any of these beautiful places in the world somewhere, where you always wanted to go, but maybe you can’t because it’s too far. To spend time with your family, your friends, you need to choose what is possible to do in one week. Also it gives you pressure okay maybe my choices are not the best one.
Mia: yeah you feel the performance anxiety for what you do in you one week
al: or maybe people have more interesting ideas than me?
Mia: i remember you also said for example they’d given you a certain chance that you might be in a wheelchair after surgery
al: a wheelchair or so like pocket for your shit if they need to cut me a part of the intestines,
Mia: yeah quite some realities. And that paper is also quite, how do you say, like a testimony of that time perspective, when you stand in the week before the surgery. You know that it’s a very specific mark of time, no?
al: yeah because it was like okay one week, it is seven days okay, too much pressure too much pressure and i will probably not sleep enough and actually it is not good before surgery you need to really be in a good physical form, you must build up your health … and also i was with no medicine anymore since a certain period. I can’t go on a massive party, or i can’t really drink alcohol…
It is also that, the time, that is really different, i still always have this pressure that i can die anytime because they maybe want to stop my medicine because it is too much side effects or they will say that my cancer is redeveloping or is it that my blood test are not good enough to continue it… today, after this conversation, I will also go to a medical appointment, and i have no idea what they will say to me.
Like for every medical appointment that i have had since the 26 December 2012,
it is all the time this suspension of time, to wait for the results and see what’s next.
There is this thing, okay, i can of course go out of this building and have a car accident, but with a disease like this it is a different time perspective, i know that i have something in me that can destroy me everyday from the inside, something that i can die from anytime
yeah I’m doing a lot of stuffs because i don’t know how much time i still have so it is because of that that everything is exciting to me. Like okay, there is this happening, yes! for sure! - and people say yeah but you know it will happen again, a next time
but me I’m like what is this next time, the next time is now, i don’t know the next time where i will be.
Mia: do you think that it started to impact your personality ? like you say it’s the reason why you very excited about things happening, and i think this is something that a lot of your friends will recognize as a sort of part of your personality, your excitement for you doing things together and building things and ah let’s go! let’s do it,
let’s do things that are… instead of just hanging around, let’s make something let’s do something, that is yeah!
al: hehe yeah but i feel tired a bit also, because i can’t release it in a way, release a bit of this pressure of time
after that surgery,
as the doctor says it was a miracle when i woke up from the surgery and he arrived to me, with a big smile. He is flemish, a little bit old and was not really a smilling guy more a person with no expression on the face, neutral.
he said yeah we succeeded alright
50:14
we succeed on what we wanted to do
and the surgery went super smooth and
and he said we put away your liver and we put it back and we open you and there was three or four surgeons around me, a gastric, a pneumo, ovarian cancer surgeon and a supervisor,
they did this radical hysterectomy,
(https://cancer.ca/en/treatments/tests-and-procedures/hysterectomy)
to remove your reproductive system, i hate this word, (the uterus, cervix, both ovaries, both fallopian tubes, and nearby tissue are removed) and the tumor, they clean everything in my belly, they clean my pleura and put a talc on it, to stop the possibility that the metastasis liquid to pass again in my pleura and compress my lung.
and this surgery was for five hours or something
and
i woke up and he said all fine,
and me, i was lying on that bed with these fifty-two staples,a long vertical line on my body,
with no possibility of moving,
i dont know why but i associated these fifty-two staples with fifty-two weeks, that is a year…
and yeah again i enter
a new perspective of lifetime
but yeah the week before that that was crazy and I was doing so many things and so my time was extended and people couldn’t follow me and they say okay you go for your party now and go for building your tree house, etc but we’re not following all of that with you because we need to sleep…..
but also it’s bizarre because that week i saw people or my friends and i said to them okay, i will have a surgery in four days five days six days (depending on when i was meeting them) but it will be my surgery of life or death and they still remember this now and
they say that for them, it also marked something in their life and they remember the time when i said it to them or what they were doing at that moment…
the time is really …. oooh
Mia: yeah this is also something about the perspective because it is suddenly different, even though the whole story, your whole trajectory is about life and death of course, but at that point it becomes very pointed. It is very right here, i dont know, the whole story could end here.
al: and pointed because of a disease that really you don’t want and it’s bizarre
that the strongest thing in your life are so connected with something that you didn’t want, something invasive and something that is still in you and that you still need to fight for or …
to fight against
Mia: after the surgery how is, how is it in them that your health and with dealing with the hospital, because it has been probably quite a gear change?
al: yeah, through these last eleven years, i had also other surgeries for the same disease but it created a lot of side effects and then i had surgeries for other parts of my body, I needed to stay at the hospital for some times but now it was the surgery for living
and what now, and what now, what now,
now i have a new perspective that i will start with a new medicine but also i was thirty-five years old and i was entering in the artificial menopause and all the side effects that comes with that.
and they said now after this surgery, you are in this new diagnosis, which is to take a medicine that we will give you on compassionate use (https://www.cancer.gov/publications/dictionaries/cancer-terms/def/compassionate-use). For 4 years more or less, i took it two times a day (with 12hours inbetween ) and i must be fasting two hours before and one hour after taking it.
Since more or less one year i take it only once a day, this was also again a big change in my life because before my day was really regulated by the moments that i was taking the treatment and fasting…
…I’m all the time in that moment of ‘soigner’ and I’m never in the curing status
because there is a difference between ‘guérir’ et ‘soigner’, to cure and treat (care for?), i dont know the exact translation in english…. i’m in an incurable illness.
(Mia: we can look it up later)
because I’m still on medication, because they give me this medication after the surgery simply because they don’t know what will happen if i don’t take it,
they don’t know
if there is still little, little things (metastasis) and so little that they can not see on the scanner then they don’t know if this little things can wake up and give me cancer again.
so they prefer to still give me this medicine,
to be, in a certain way, sure that they tried something and that something will not wake up again,
and me, i needed to agree to this choice also, to continue to be on medication or to stop because i was feeling that it was too much, too many years of treatments.
Part 7 - LIMBO
Mia:
you’re in this reality where
you are kind of treated as a cancer survivor,
how do you say,
that you beat the cancer
but you are still on medication to make sure that it doesn’t come back.
al:
they said they would give it to me until i have too many side effects, they want to give it as long as they can
and as long as they can means; either i have too many side effects and i can’t live my life properly or the cancer is growing again because at a certain point it’s been five years that i take this medicine and your body at a certain time takes the habit of a medicine, so it doesn’t work anymore and it doesn’t understand if you are taking something or not.
59:00
so it is this time that
you don’t know
and now i’m in the time where we don’t know if the side effects that i have right now are from the medicine or not, we are not sure of that, and it is the test that we are doing these last years because it became bigger side effects.
And today this is what we will discuss at the hospital, it’s been four months that i really don’t feel good at the beginning of taking the medicine, i could surpass the pain, right now i have this big dermatitis, skin disease on my finger, i have this golden staphylococcus on my fingers, i can’t use my hands anymore, and they gave me creams, cortisone, etc but nothing changes probably because i still take the medicine, so it is a loop of the medicine creating this.
I went at the hospital like ten times these last months, trying to know what to do and what i have, but there was no clear answer, or some unclear propositions coming from differents doctors but nothing changed,
and so i really said to them like beginning of June, we meet all together and take a decision on which tests we are doing or which protocols I’m entering in because now i feel that i can’t be in this loop of time again, where i’m coming back at the hospital every month.
This is the kind of hardcore limbo where there is no horizon
yeah yeah because for now i dunno if it’s good to take the medicine or not, if the side effects are there all the time. i dunno if it’s good that i put this cortisone cream on my hands every day, if it’s good or not but for my body, i feel by myself that is not good,
I’m also tired
because in these eleven years, i’m 40 years old now, you are not the same patient, you start really to know how it works and you start to know your body,
it became a kind of routine every time that i go at the hospital, you have your appointment, the nurse come, do the blood test, do the CTscan and the echography, you wait, one hour, two hours, three hours, 5, 6 hours, and after every time you go you have a different doctor that comes to ask you how you feel, it goes fast with them, it is the between that takes so long, they listen a bit your side effects but don’t have real solution for you, you receive you medicine and you go home and…
you become a machine, a ghost, a patient but not really a human,
in that place
also because it was a long time that i’m there and that feeling i really don’t like it because I still need to continue my life …
and now we are there again…
i think for me for now, we don’t have any perspective because at my last appointment I know that they don’t have any other medicine to give me so i don’t know what will happen if the side effects on my hands don’t decrease and the only solution probably is to stop the medicine …
and i need probably to make that decision today, like this afternoon,
do i still continue this medicine and have the side effects that are really not good,
or do i stop it?
but this is a super huge decision because i have no idea if my cancer cells will redevelop if i stop
so yeah right now we are in this time perspective of some hours
i have my appointment today at the hospital at 3:30 PM
Mia: maybe it would be nice to have another conversation, if you would be up for it? it doesn’t have to be instantly, it can be in a couple of weeks or something to talk a bit again cause, i dunno, maybe that’s a nice place to end the recording, in terms of … it’s now been an hour.
=================================
PICTURES